Have you ever wondered what causes varicose veins to appear or why your legs feel so heavy and achy at the end of the day? While many people attribute these issues to aging or long hours on their feet, the real culprit is often a specific medical phenomenon known as venous reflux. This condition is the starting point for nearly all forms of chronic vein disease, setting off a chain reaction that can lead to significant discomfort and health complications.
Understanding venous reflux is the key to understanding your leg health. It explains why simple symptoms can escalate over time and why effective treatment must target the root of the problem, not just the visible signs. In this detailed guide, we will demystify the concept of venous reflux, explore how this backward blood flow leads to chronic vein disease, and discuss the modern treatment options available. For those experiencing vein symptoms in legs, this knowledge is the first step toward finding lasting relief with a top vein specialist Manhattan.
The Basics of Healthy Blood Circulation in the Legs
To learn more about the conditions affecting vein health, visit our chronic vein conditions resource.
Before we can explore what goes wrong, it’s essential to understand how your leg veins are designed to function. Your circulatory system is a continuous loop. Arteries carry oxygen-rich blood from your heart down to your extremities, including your legs and feet. Veins have the much more difficult job of returning that deoxygenated blood back up to the heart, working directly against the force of gravity.
To accomplish this impressive feat, your leg veins rely on a sophisticated two-part system:
- The Calf Muscle Pump: Your leg muscles are the primary engine for your venous system. As you walk, run, or even flex your ankles, your calf muscles contract and squeeze the deep veins embedded within them. This powerful squeezing action propels blood upward, pushing it segment by segment toward the heart.
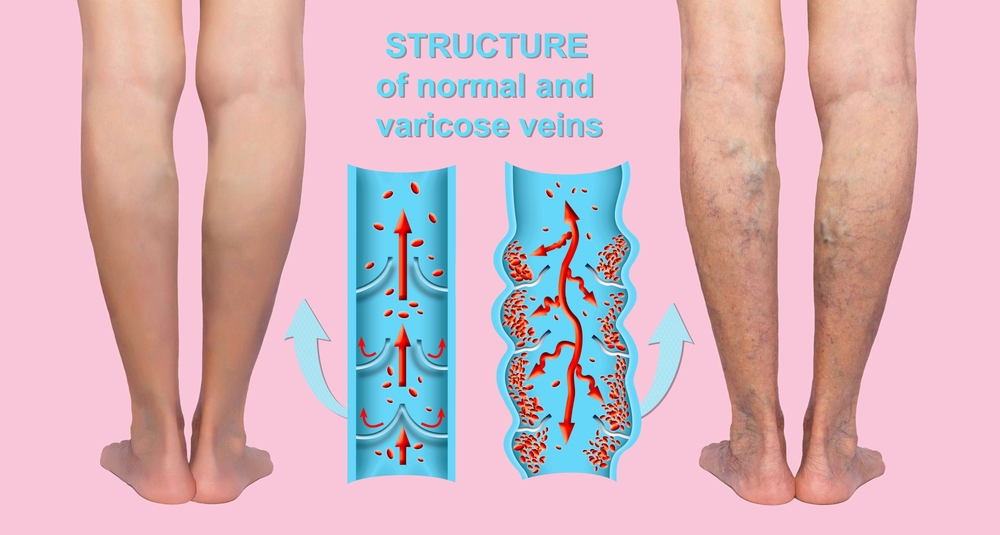
- One-Way Venous Valves: Situated every few inches inside your veins are tiny, delicate flaps of tissue called valves. These act as one-way doors. When the calf muscles pump blood upward, the valves open to let the blood pass through. When the muscle relaxes and gravity tries to pull the blood back down, the valves snap shut, preventing any backward flow.
This elegant system ensures that blood flows in a single direction: up. When both the muscle pump and the valves are working correctly, circulation is efficient, and your legs feel light and pain-free.
What is Venous Reflux?
Venous reflux, also known as venous insufficiency, is the medical term for what happens when this system breaks down. (You can learn more about various chronic vein conditions here.) Specifically, it refers to the failure of the one-way venous valves. When these valves become damaged, weakened, or “incompetent,” they no longer form a tight seal.
Venous reflux, also known as venous insufficiency, is the medical term for what happens when this system breaks down. Specifically, it refers to the failure of the one-way venous valves. When these valves become damaged, weakened, or “incompetent,” they no longer form a tight seal.
Instead of snapping shut to block the downward pull of gravity, the faulty valves allow blood to leak backward and flow in the wrong direction. This blood then pools in the lower portions of the veins, typically in the calves and ankles. This process of backward flow and pooling is the definition of venous reflux. It is not a disease in itself but rather the underlying mechanical failure that causes chronic vein disease.
What Causes Valves to Fail?
Venous valves are delicate structures, and several factors can contribute to their damage over time:
- Genetic Predisposition: This is the most common cause. Many people inherit veins with weaker walls or inherently less robust valves, making them more susceptible to failure. If your parents had varicose veins, you have a significantly higher risk.
- Age: Over decades of use, valves can simply wear down, losing their flexibility and ability to close tightly.
- Hormonal Factors: Hormones like progesterone, which fluctuate during pregnancy and menopause, can cause the vein walls to relax and stretch. This stretching can pull the valve flaps apart, creating a gap that allows for reflux.
- History of Deep Vein Thrombosis (DVT): A blood clot in a deep vein can cause inflammation that permanently scars and damages the valves, even after the clot is gone. This is known as post-thrombotic syndrome.
- Lifestyle: While less of a direct cause of valve failure, lifestyles involving prolonged periods of standing or sitting can exacerbate the problem by allowing blood to remain stagnant in the legs for long periods, putting continuous stress on the valves.
The Cascade of Damage: How Reflux Leads to Chronic Vein Disease
If you’d like to read more about these underlying vein disorders, be sure to visit our dedicated chronic vein conditions resource for more detailed information.
Venous reflux isn’t a static event. Once it begins, it initiates a destructive cycle that causes symptoms to appear and progressively worsen. The entire spectrum of chronic vein disease can be traced back to the consequences of this backward blood flow.
Venous reflux isn’t a static event. Once it begins, it initiates a destructive cycle that causes symptoms to appear and progressively worsen. The entire spectrum of chronic vein disease can be traced back to the consequences of this backward blood flow.
Stage 1: The Onset of Venous Hypertension
The immediate consequence of venous reflux is the pooling of blood in the lower leg veins. This stagnant blood dramatically increases the pressure inside these vessels. This condition is called venous hypertension, and it is the central engine driving all subsequent symptoms and complications. A healthy leg vein has very low pressure, but in a leg with significant reflux, the pressure can become extremely high, especially after standing for a long time.
Stage 2: Vein Distention and the Formation of Varicose Veins
Vein walls are elastic, but they are not designed to withstand the constant high pressure of venous hypertension. Under this relentless force, the vein walls begin to stretch, weaken, and lose their tone. As they stretch, they become longer and wider.
This is what leads to the formation of varicose veins. The veins twist and contort to accommodate their new, longer length within the same physical space, creating the bulging, rope-like appearance visible on the skin’s surface. A small, barely visible vein can transform into a large, prominent varicose vein as venous hypertension continues to stretch it year after year. This process also creates a vicious cycle: as the vein wall stretches, it pulls the already-faulty valve leaflets even further apart, worsening the reflux and leading to even higher pressure.
Stage 3: The Emergence of Pain and Discomfort
The high pressure and stagnant blood trigger an inflammatory response in the vein walls and surrounding tissues. This chronic inflammation is the source of many of the classic vein symptoms in legs.
- Aching and Heaviness: The pressure and inflammation cause a dull, throbbing ache and a sensation of heaviness or fatigue in the legs.
- Cramping and Restless Legs: The buildup of metabolic waste products in the stagnant blood can irritate nerves and muscles, leading to painful night cramps and the uncomfortable sensations of Restless Legs Syndrome.
These symptoms are a direct result of the physiological stress caused by venous reflux and hypertension. They are often worst at the end of the day, after hours of gravity taking its toll, and are relieved by elevating the legs, which helps drain the pooled blood and reduce the pressure.
Stage 4: Fluid Leakage and Swelling (Edema)
As the pressure inside the veins continues to rise, it eventually exceeds the pressure in the surrounding tissues. This pressure gradient forces fluid to leak out of the microscopic capillaries and into the interstitial space—the tissue around the blood vessels.
Initially, this leakage is minor, causing slight swelling (edema) in the ankles that might only be noticeable in the evening. However, as the reflux worsens and the venous hypertension becomes more severe, the leakage increases. The lymphatic system, which is responsible for clearing excess fluid, becomes overwhelmed. The swelling becomes more pronounced and persistent, affecting the entire lower leg and no longer resolving completely overnight.
Stage 5: Skin Damage and Discoloration
Chronic venous hypertension has a devastating effect on the health of the skin, particularly around the ankles where the pressure is highest.
- Stasis Dermatitis: The constant inflammation and poor circulation lead to a skin condition called stasis dermatitis. The skin becomes itchy, red, and may even “weep” a clear or yellowish fluid.
- Hemosiderin Staining: The high pressure forces red blood cells out of the capillaries and into the skin tissue. As these cells break down, they release iron pigment (hemosiderin), which permanently stains the skin a brownish or reddish-rust color. This discoloration is a clear visual sign of advanced vein disease.
- Lipodermatosclerosis: Over years, the chronic inflammation can lead to the formation of scar tissue in the fatty layer beneath the skin. This causes the skin to become hard, woody, and painfully tight. This condition, known as lipodermatosclerosis, makes the skin extremely fragile.
Stage 6: The Formation of Venous Ulcers
This is the final and most severe consequence of untreated venous reflux. The skin has become so damaged, malnourished, and inflamed that even a minor injury, like a scratch or a bump, cannot heal. The tissue breaks down, creating an open sore known as a venous ulcer.
These ulcers typically form on the inner ankle, an area known as the “gaiter region.” They are notoriously difficult to heal because the underlying circulatory problem—venous reflux and hypertension—prevents the delivery of the oxygen and nutrients needed for tissue repair. Venous ulcers can cause significant pain, are prone to infection, and can dramatically reduce a person’s quality of life.
How is Venous Reflux Diagnosed?
Learn more about chronic venous conditions and diagnostic options at our Manhattan vein treatment center.
Given that venous reflux is the root cause of these issues, identifying it is the most critical step in diagnosis. If you’re searching for a “chronic vein condition specialist near me,” you should look for a physician who uses duplex ultrasound for diagnosis.
A duplex ultrasound is a non-invasive, painless imaging test that is the gold standard for diagnosing venous reflux. It allows the specialist to:
- Visualize the Veins: The ultrasound creates a real-time map of your superficial and deep leg veins.
- Measure Blood Flow: The “duplex” part of the scan uses Doppler technology to measure the direction and speed of blood flow within the veins.
- Test Valve Function: The technician will squeeze your calf to simulate the muscle pump and then release it. By watching the screen, the specialist can see if blood flows backward through the valves when the calf is released. This directly visualizes and confirms the presence of venous reflux.
- Rule Out Other Issues: The scan can also identify other problems, such as blood clots (DVT).
This detailed diagnostic information allows a vein specialist to pinpoint exactly which veins and valves are failing, determine the severity of the reflux, and create a highly targeted treatment plan.
Treatment: Correcting Venous Reflux at the Source
To learn more about specific chronic vein conditions and the full scope of modern treatment options, visit our chronic vein conditions page.
Since venous reflux is a mechanical problem, the most effective treatments work by eliminating the pathway for backward blood flow. Modern vein care treatment Manhattan focuses on closing or removing the diseased veins that have incompetent valves. When a faulty vein is closed, the body’s circulatory system automatically reroutes blood to the many other healthy veins in the leg, restoring normal upward flow and immediately resolving the venous hypertension.
The most common and effective minimally invasive procedures include:
Endovenous Thermal Ablation (EVLT or RFA)
This is the leading treatment for reflux in the large saphenous veins, which are often the primary sources of varicose veins.
- The Procedure: Under local anesthesia, the vein specialist Manhattan uses ultrasound to guide a thin laser fiber (EVLT) or radiofrequency catheter (RFA) into the diseased vein. The device is activated, delivering controlled heat that seals the vein shut from the inside.
- The Result: The treated vein is gradually absorbed by the body. Blood flow is redirected to healthy veins, the venous pressure drops, and symptoms like pain, swelling, and varicose veins resolve.
Sclerotherapy
Sclerotherapy is ideal for treating smaller varicose veins and spider veins.
- The Procedure: A medicated solution called a sclerosant is injected directly into the target vein. This solution irritates the vein lining, causing it to scar and close off.
- Ultrasound-Guided Sclerotherapy: For larger, deeper veins that are not suitable for thermal ablation, the specialist can use ultrasound to guide the sclerosant injection for precise delivery.
Ambulatory Phlebectomy
This procedure is used to physically remove large, bulging varicose veins that are close to the surface of the skin. It is often performed in conjunction with an ablation procedure that closes the underlying source vein.
Venous reflux is the definitive starting point of a long and predictable journey of decline in your leg health. What begins as a minor valve leak can, over time, lead to debilitating pain, swelling, and skin damage. The good news is that this process is both identifiable and treatable. By understanding that your symptoms are likely caused by this underlying mechanical failure, you can seek the right kind of help. A proper diagnosis and a modern, minimally invasive treatment can correct the reflux, break the cycle of venous hypertension, and restore your legs to health.
Leading Manhattan Vascular & Vein Specialist
At Fox Vein Care, we provide state-of-the-art vascular and venous treatments, combining advanced diagnostic technology with minimally invasive procedures that prioritize comfort, safety, and outstanding results.
Contact Us

